Accurate fetal heart rate (FHR) assessment may help in determining the status of the fetus and indicate management steps for a particular condition. In order to accurately assess a FHR pattern, a description of the pattern should include qualitative and quantitative information in the following five areas:
- Baseline rate
- Baseline FHR variability
- Presence of Accelerations
- Periodic or episodic decelerations
- Changes or trends of FHR patterns over time
These areas include fetal heart rate patterns with specific definitions and descriptions. These definitions and descriptions are the terminology used by the National Institute of Child Health and Human Development and have been adopted by the American College of Obstetrics and Gynecology (ACOG) and the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN).
To appropriately interpret a fetal monitoring tracing, the systematic approach below should be followed:
- Evaluate the recording: is it continuous and adequate for interpretation?
- Identify the type of monitor used – external versus internal: second generation versus first generation.
- Identify the baseline fetal heart rate and presence of variability.
- Determine the presence of accelerations or decelerations from baseline.
- Identify changes or trends in FHR patterns over time
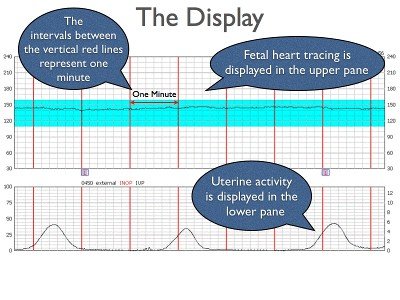
In addition to monitoring fetal heart rate patterns, information about the effects of labor on the fetus can also be learned by observing the pattern of uterine contractions. Uterine contraction patterns can provide information about the progress of labor. Also, because uterine contractions can affect placental exchange, evaluation of contraction patterns may provide clues as to the potential effects of the contraction rate and force on the fetus.
Uterine contractions are dealt with at the end of this section.
Demonstrated below is a picture from a typical EFM display and a sample EFM strip.
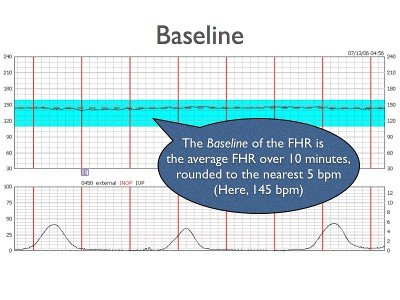
Baseline
The mean FHR rounded to increments of 5 beats per min during a 10 min segment, excluding:
- Periodic or episodic changes
- Periods of marked FHR variability
- Segments of baseline that differ by more than 25 beats per min
- The baseline must be for a minimum of 2 min in any 10-min segment (NICHD)
In order to determine whether there are changes in the fetus’ physiologic status, a baseline heart rate must first be determined as a reference. All changes are therefore, based on a deviation from that fetus’ resting norm.
The normal FHR baseline should range between 110 beats/min to 160 beats/min. The baseline FHR is normally set by the atrial pacemaker and the beat-to-beat differences in the heart rate are governed by a balance between the sympathetic and parasympathetic branches of the autonomic nervous system.
As the central nervous system matures, the baseline FHR gradually drops, and the normal ranges for a mid-trimester fetus are between 150-170 beats/min. Parasympathetic tone becomes more dominant with advancing gestational age, and a post-term fetus may have a FHR between 110-120 beats/min.
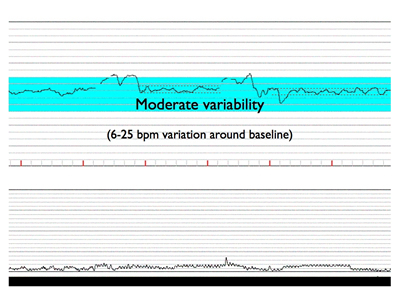
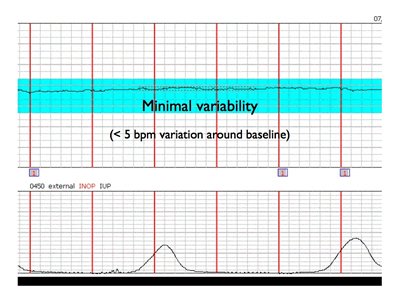
Baseline Variability
- Fluctuations in the FHR of 2 cycles per min or greater
Baseline Variability- Variability is visually quantitated as the amplitude of peak-to-trough in beats per min
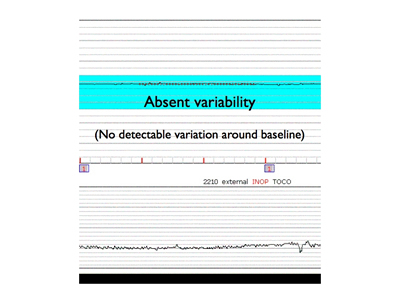
- Absent: amplitude range undetectable
- Minimal: amplitude range detectable but 5 beats per min or fewer
- Moderate (normal): amplitude range 6-25 beats per min
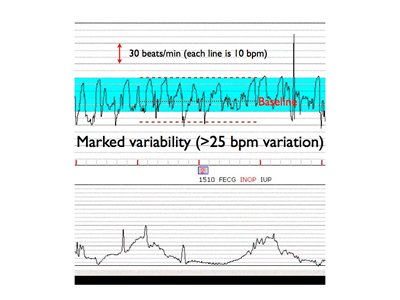
- Marked: amplitude range greater than 25 beats per min (NICHD)
In the normal fetus, there is an interplay between the sympathetic (acceleration) and parasympathetic (deceleration) nervous systems in the control of heart rate. These systems exert their control via the cerebral cortex, the medulla oblongata, the sympathetic ganglia and the vagus nerve. The interaction between these systems results in a difference in the beat-to-beat intervals resulting in variability of the fetal heart rate tracing. In the term fetus, moderate variability is considered normal as it indicates a normally functioning central nervous system. Conditions that alter the integrity of this neuro-cardiac axis, such as hypoxemia, result in loss of heart rate variability. Variability therefore, is the single most important indicator of an adequately oxygenated fetus. Below is example of moderate variability.
Decreased or absent variability therefore represents some dysfunction in one or both of these systems, or in increased and dominant tone of one system over the other, such as during sleep cycles or due to the effects of drugs.
Causes of decreased variability include:
- Hypoxemia/acidosis
- Fetal sleep cycles
- Drugs (Analgesics, barbiturates, tranquilizers, phenothiazines, para-sympatholytics, anesthetics)
- Prematurity
- Arrhythmias
- Fetal tachycardia
- Preexisting neurological abnormality
- Congenital anomalies
Below is an example of minimal variability.
 Here is an example of absent variability:
Here is an example of absent variability:
Marked variability in the baseline FHR is present when the amplitude exceeds 25 BPM.This pattern (sometimes called a saltatory pattern) suggests acute hypoxia or mechanical compression of the umbilical cord and is often seen during the second stage of labor. When coupled with decelerations, this pattern is considered non reassuring and should warn the physician to search for, and correct, potential causes of hypoxia. Causes of marked (increased or saltatory) variability include:
- Fetal stimulation
- Mild, transient hypoxemia
- Drugs
Here is an example of marked variability:
 Two types of variability have also been described prior to the NICHD definitions. Short term variability (STV) describes the beat-to-beat fluctuations in the FHR measured from R wave to R wave by fetal ECG. Long term variability (LTV) represents the amplitude changes of the normal baseline over time, with a cyclic changes occurring in less than one minute.
Two types of variability have also been described prior to the NICHD definitions. Short term variability (STV) describes the beat-to-beat fluctuations in the FHR measured from R wave to R wave by fetal ECG. Long term variability (LTV) represents the amplitude changes of the normal baseline over time, with a cyclic changes occurring in less than one minute.
The NICHD does not distinguish between LTV and STV, because they are viewed as a unit when the FHR is visually analyzed. Additionally, LTV and STV generally respond synchronously in response to changes in autonomic tone, and thus differentiation between LTV and STV generally does not provide additional information regarding the fetal oxygenation. There are some special circumstances where this not true; for example, a fetus with severe anemia demonstrates a pattern with absent STV but present LTV. This unique tracing is referred to as a sinusoidal pattern and will be discussed separately.
Acceleration
A visually apparent increase (onset to peak in less than 30 sec) in the FHR from the most recently calculated baseline
- The duration of an acceleration is defined as the time from the initial change in FHR from the baseline to the return of the FHR to the baseline
- At 32 weeks of gestation and beyond, an acceleration has an acme of 15 beats per min or more above baseline, with a duration of 15 sec or more but less than 2 min
- Before 32 weeks of gestation, an acceleration has an acme of 10 beats per min or more above baseline, with a duration of 10 sec or more but less than 2 min
- Prolonged acceleration lasts 2 min or more, but less than 10 min
- If an acceleration lasts 10 min or longer, it is a baseline change (NICHD)
Accelerations of the FHR may be periodic (that is, occurring in relation to a contraction) or episodic (no association with a contraction). Most are episodic. These episodic accelerations are generally in response to fetal movement, with a need for increased perfusion, and therefore transiently increased sympathetic tone, or due to fetal stimulation, such as scalp stimulation with a vaginal exam, abdominal palpation, or vibroacoustic stimulation.
Periodic accelerations are those associated with uterine contractions and may be due either to fetal stimulation (particularly in breech presentation) or due to mild cord compression (that is, compression of the umbilical vein only).
FHR accelerations and good (moderate) variability are closely associated and sometimes may be visually indistinguishable, though both are reflective of a well-oxygenated fetus.
The presence of accelerations forms the basis of the nonstress test (NST). An NST is said to be reactive when there are at least two accelerations in a 20 minute period, along with moderate variability and no decelerations.
Below is an example of fetal acceleration:
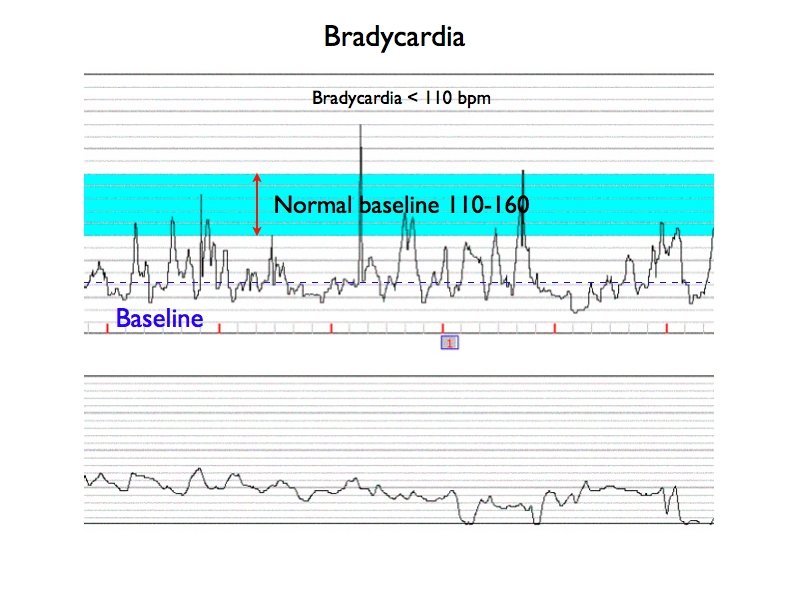
Bradycardia
Baseline FHR less than 110 beats per min (NICHD)
Fetal bradycardia is commonly associated with fetal hypoxemia. However, a number of causes must be considered:
- Hypoxemia
- Drugs
- Maternal hypotension
- Hypothermia
- Maternal hypoglycemia
- Fetal bradyarrhythmias
- Complete heart block (Maternal SLE, CMV infection)
- Congential heart block
- Umbilical cord compression
- Amniotic fluid embolism
- Normal variation
As with fetal tachycardia, the bradycardic FHR must be analyzed for the presence of periodic changes and decreased variability. These findings are more consistent with hypoxemia. Some fetuses may display a bradycardic FHR but be completely normal. It should be remembered that the range of 110-160 does not represent all normal fetuses. The likelihood of a FHR in the range of 100-110 representing a normal variant increases as the fetus, and its nervous system, matures.
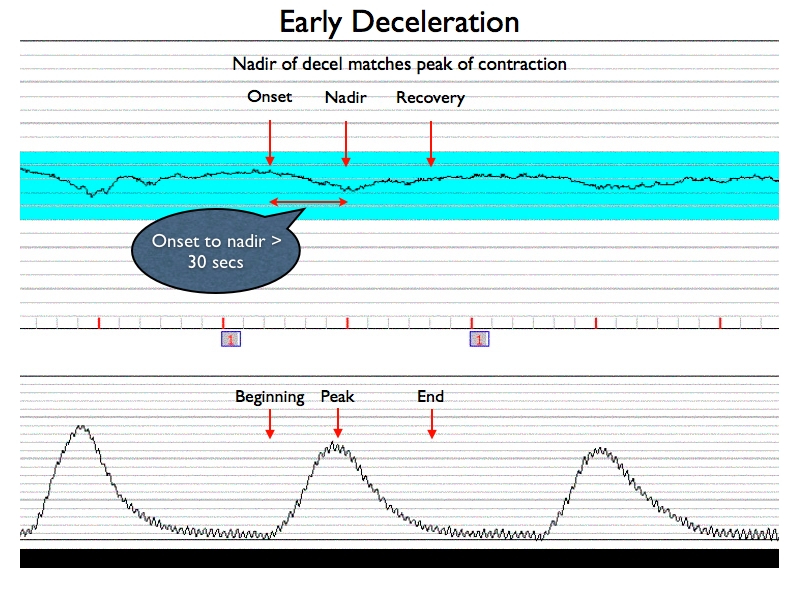
Early Deceleration
- In association with a uterine contraction, a visually apparent, gradual (onset to nadir 30 sec or more) decrease in FHR with return to baseline
- Nadir of the deceleration occurs at the same time as the peak of the contraction (NICHD)
An early deceleration and a late deceleration may visually appear identical. Both are smooth and curvilinear and appear to be a mirror image of the contraction. The distinction between the two is based upon the relationship of the deceleration to the uterine contraction (UC).
Early decelerations correspond, temporally, to the contraction and therefore exist only as a periodic change. Early decelerations are a benign finding caused by a vasovagal response as a result of fetal head compression by the contraction. Pressure on the fetal skull alters the cerebral blood flow and this in turn stimulates the vagus nerve. The heart rate is gradually decreased as the pressure of the contraction intensifies, and the deceleration gradually resolves as the pressure resolves. This pattern is generally limited to the active stage of labor. If the pattern is found in early labor, it may be associated with cephalopelvic disproportion (CPD).
Early decelerations have not been associated with fetal hypoxemia or acidosis.
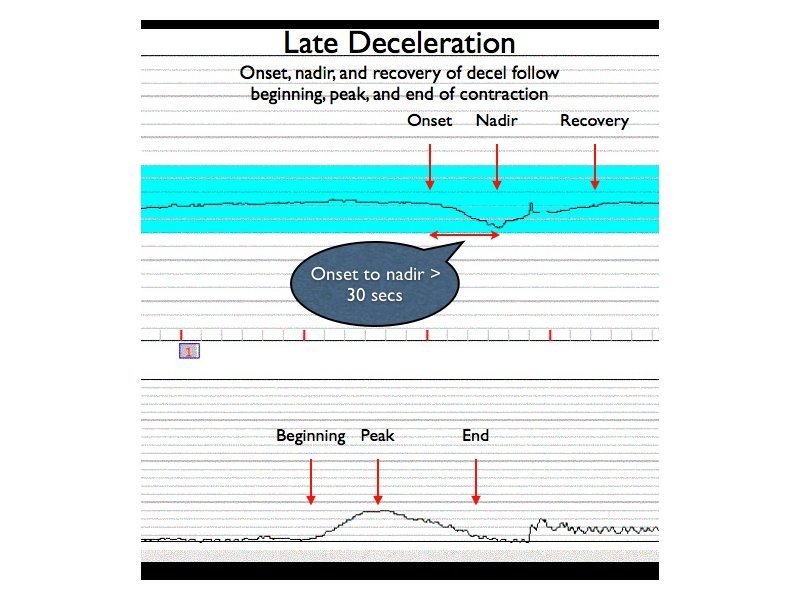
Late Deceleration
- In association with a uterine contraction, a visually apparent, gradual (onset to nadir 30 sec or more) decrease in FHR with return to baseline
- Onset, nadir, and recovery of the deceleration occur after the beginning, peak, and end of the contraction, respectively (NICHD)
Though late decelerations share the same morphologic shape as early decelerations, they tend to appear late, after the onset and nadir of the contraction.
Two varieties of late decelerations have been described, reflex and nonreflex. Reflex late decelerations are those which occur in the presence of normal FHR variability, whereas non-reflex late decelerations occur in association with diminished or absent FHR variability.
The classically described cause of late decelerations is uteroplacental insufficiency (UPI). In UPI, there may be a problem with a uterine perfusion or uterine activity or there may be a problem with the placenta, or both.
Uterine hyperactivity is associated with decreased time for intervillous space blood flow between uterine contractions. Similarly, maternal hypotension, even in the presence of normal uterine activity, will result in decreased volume of the intervillous space blood flow. Either of these factors may lead to a decrease in the maternal-fetal oxygen transfer.
Placental dysfunction, too, may lead to a decreased maternal-fetal oxygen transfer, and/or a smaller volume of placental reserve in proportion to fetal need.
Any of these causes may eventually lead to fetal hypoxemia and eventually myocardial depression. A vasovagal reflex leads to cardiodeceleration and continued hypoxemia may lead to lactic acidosis secondary to anaerobic metabolism.
Reflex late decelerations are thought to be due to vagal stimulation by chemoreceptors in the head in response to low oxygen tension. This is accentuated by the decreased oxygen transfer during a uterine contraction. The hypoxemia results in increased sympathetic stimulation leading to increased systemic vascular resistance. The response to this increased pressure is a vagally mediated decrease in heart rate. This dual reflexive response may explain the delay in the heart rate following a contraction. Reflex late decelerations are associated with normal FHR variability because CNS system is intact.
Nonreflex late decelerations, however, are associated with decreased or absent FHR variability. These decelerations are associated with a greater degree of relative hypoxemia and result in hypoxic depression of the myocardium coupled with the previously described vagal response. In reflex late decelerations, variability was maintained because the fetus was able to compensate, shifting oxygenated blood to vital organs (e.g., the heart), but in nonreflex late decelerations, the fetus is unable to compensate. It is these late decelerations which are more typically associated with fetal acidosis, and they are more commonly associated with placental dysfunction rather than uterine hypoperfusion or hyperactivity.
The causes of UPI are varied, and many are reversible:
- Uterine hyperactivity
- Maternal hypotension
- Maternal hypertensive disorders
- Placental abruption
- Placenta previa
- IUGR
- Maternal DM
- Chorioamnionitis
- Postterm gestation
- Maternal anemia, SS anemia, etc.
- Rh isoimmunization
- Maternal cardiac disease
- Maternal smoking
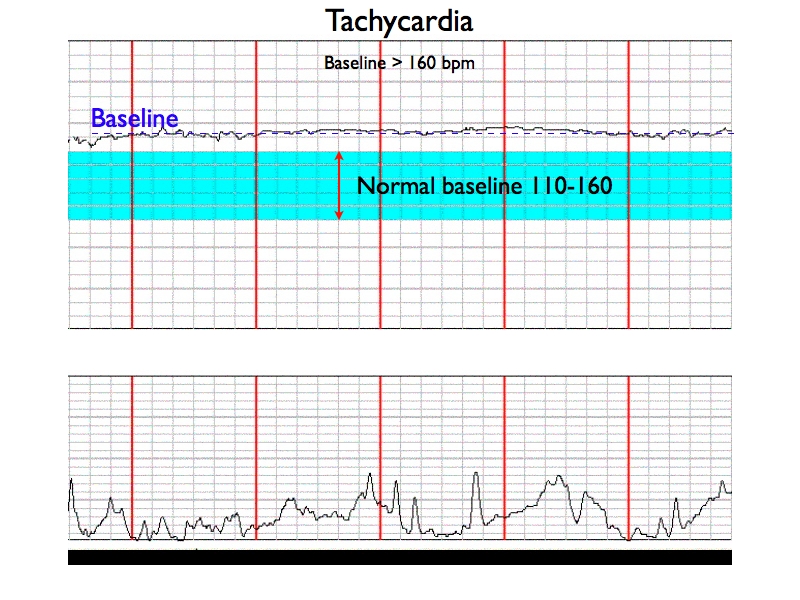
Tachycardia
Baseline FHR greater than 160 beats per min (NICHD)
There are several causes of fetal tachycardia that must be considered, including:
- Maternal fever
- Chorioamnionitis
- Fetal sepsis
- Drugs (Atropine, Vistaril, Phenothiazines, Beta-sympathomimetics)
- Fetal hypoxemia
- Tachyarrhythmias
- Fetal heart failure
- Severe fetal anemia, fetal hydrops
- Maternal hyperthyroidism
In general, tachycardia from any cause is related to an increase in sympathetic tone and/or a diminishment of parasympathetic tone. This means that one would normally expect an overall decrease in variability in association with tachycardia.
Fetal tachycardia is occasionally seen after a deceleration of the FHR, and in this instance is likely indicative of hypoxemia. This may be due to an attempt by the fetus to increase perfusion by increasing cardiac output or it may be due to increased catecholamine activity from the adrenal medulla in response to the stress of hypoxemia, when associated with a deceleration, and the loss of vagal tone.
Because the mechanisms for tachycardia related to hypoxemia are predisposed by some other signal hypoxic event, such as a prolonged deceleration, then isolated tachycardia, without evidence of periodic changes and in the presence of normal, though slightly diminished variability, is almost always due to a cause other than hypoxemia. Fever and/or chorioamnionitis are very common causes and fetal tachycardia may persist up two hours after correction of maternal fever.
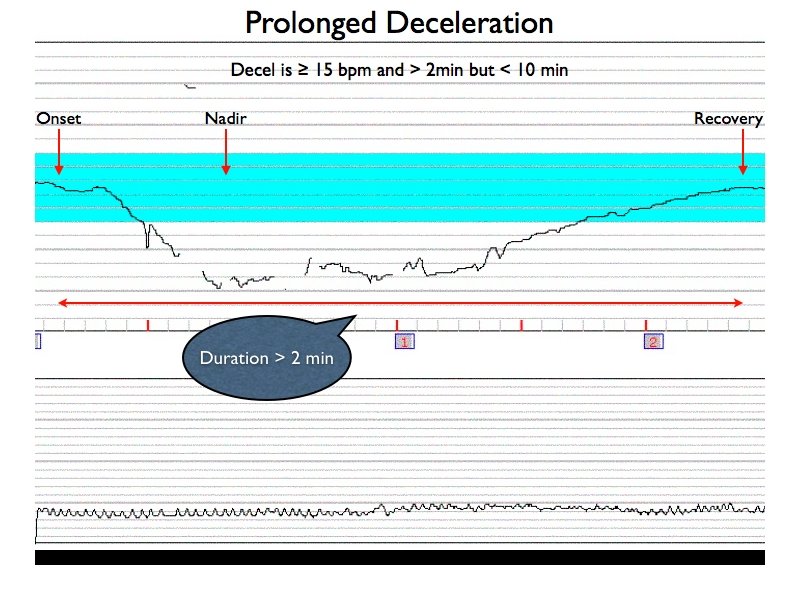
Prolonged Deceleration
- Visually apparent decrease in the FHR below the baseline
- Deceleration is 15 beats per min or more, lasting 2 min or more but less than 10 min from onset to return to baseline (NICHD)
Prolonged decelerations can be caused by any mechanism which normally may lead to periodic or episodic decelerations, but the return to baseline is delayed because the stimulus or mechanism causing the deceleration is not reversed. This often is associated with hypoxia. Mechanisms which are less likely to resolve spontaneously are therefore more likely to be associated with prolonged decelerations, such as cord compression, profound maternal hypotension or hypoxemia, tetanic uterine contractions, or prolonged head compression associated with the second stage of labor. A FHR above 100 beats/min with good variability is tolerable, but a prolonged deceleration below 100 beats/min calls for immediate efforts at resolution and a drop below 60 beats/min becomes an obstetric emergency since it is almost always associated with fetal hypoxia.
Variable Deceleration
- An abrupt (onset to nadir less than 30 sec), visually apparent decrease in the FHR below the baseline
- The decrease in FHR is 15 beats per min or more, with a duration of 15 sec or more but less than 2 min (NICHD)
Variable decelerations appear morphologically different from either early or late decelerations. They are characterized by a sudden, abrupt drop in the FHT along with usually a similarly abrupt return to baseline. The shape varies widely, and they may appear as a V, U, or W. They may be either periodic or episodic. Often, there are small accelerations immediately before and immediately following the deceleration. These associated accelerations are often referred to as shoulders.
The classic mechanism described as the cause of variable decelerations is umbilical cord compression. Initial or mild umbilical cord compression results in occlusion of the umbilical vein, which is larger than the arteries and less rigid. This results in decreased venous return resulting in reflex tachycardia to maintain cardiac output. This explains the initial increase in heart rate (shoulder) preceding the deceleration. Further compression of the cord leads to occlusion of the umbilical artery, and the resulting increased systemic resistance, sensed by the baroreceptors, results in a protective reflex slowing of the heart rate. As the cord is decompressed, this series of events is reversed, and an acceleration may follow the deceleration (artery is decompressed but the vein is still compressed) prior to returning to baseline.
Variable decelerations are classified as severe when they last more than 60 seconds, fall below 70 beats/min, or have a drop of 60 beats/min below the baseline rate.
While umbilical cord compression is typically responsible for this pattern in the first stage of labor, it may also result from head compression during the second stage of labor.
Variable decelerations may be seen in the antepartum or early in labor if associated with oligohydramnios. Similarly, they may be detected after rupture of membranes, and in this setting they may portend cord prolapse, particularly if rupture of membranes occurred prior to engagement of the presenting part. During the descent phase of labors, typically between 8-10 cm cervical dilation, variables may be associated with nuchal cords causing cord stretch or compression, or with head compression associated with rapid descent and maternal valsalva.
Variable decelerations in the presence of normal FHR variability are not thought to represent hypoxia, but repetitive severe variable decelerations with diminished or absent FHR variability may indicate hypoxia.
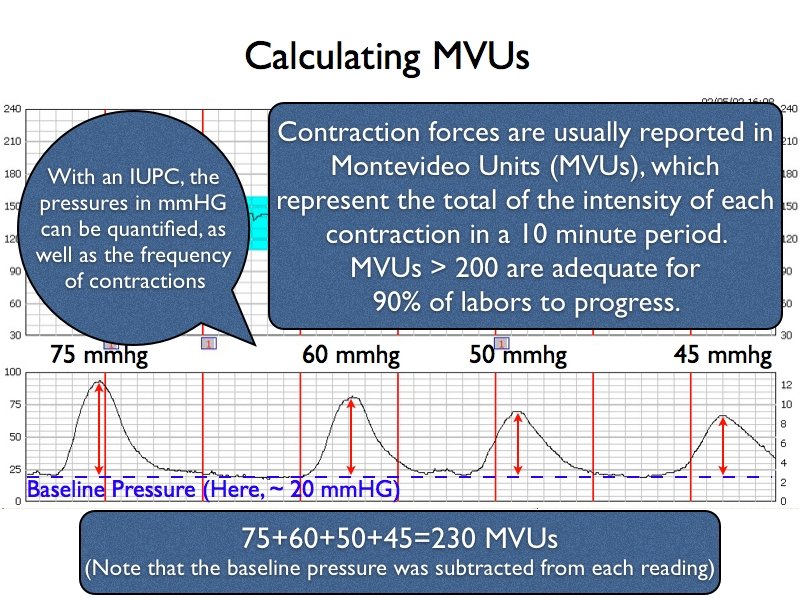
Uterine Contractions
Two types of information can be ascertained from uterine contraction monitoring: quantitation of uterine activity (the strength of contractions), and contraction patterns (e.g. how many contractions, how often they are occurring). Assessment of contraction patterns is qualitative and can be performed with an external tocodynamometer or tocotransducer (Toco), whereas quantitative measurement of uterine strength requires an internal uterine pressure catheter (IUPC).
Qualitative patterns include regular uterine contractions, polysystole, tachysystole, paired contractions, skewed contractions, tetanic contractions, and uterine hypertonus.
In most normal spontaneous labors, contractions occur with a frequency of 2-5 minutes, and they may last between 30-60 seconds. The ascent and descent of the contraction are gradual and similar to one another. Contractions tend to become stronger and more frequent as labor progresses. Such a contraction pattern would be denoted as regular uterine contractions, with a commentary on the frequency of the contractions (e.g., every 2-3 minutes).
A normal contraction pattern is demonstrated in the picture above with contractions every 2-3 minutes.
Quantitative methods include Montevideo units (MVUs), Alexandria units, Active Planimeter units, Total planimeter units, and average rate of rise. Commonly, only MVUs are used in the US outside of research protocols.
With an IUPC in place, quantitative data can be measured, most commonly using Montevideo units (MVU). A Montevideo Unit is the sum of the intensity of each contraction in a 10 minute period (in mmHG). Adequate uterine activity is defined as a contraction pattern that generates greater than 200 MVUs. Studies have shown that this threshold is adequate for 90% of labors to progress. Among women in spontaneous labors, more than 40% have MVUs > 300 mmHG. Baseline pressure, or resting tone, is the uterine pressure in mm Hg while the uterus is relaxed.
Types of Uterine Contraction Patterns
- Tachysystole (or polysystole) is defined as 6 or more UCs in 10 minutes without evidence of fetal distress.
- Hypertonus is either an abnormally high uterine resting tone (>25 mmHG) or MVUs > 400.
- Hyperstimulation is an archaic term. It is still frequently encountered in the literature and means either:
- Persistent tachystole classically with evidence of fetal distress (late decelerations, lost variability) but later accepted as even without distress (the same as modern definition of tachysystole), or
- A single UC lasting > 2 minutes which may also be called a tetanic contraction, or
- Uterine contractions occurring within one minute of each other.
The most common cause of a tachysystolic, polysystolic or hypertonic contraction pattern is oxytocin or prostaglandins.
Other contractions sometimes described:
- Paired contractions, which are contractions that are coupled together, one after the other, then a prolonged gap in uterine activity occurs before the next set of paired contractions. This is sometimes thought to indicate cephalopelvic disproportion (CPD).
- A skewed contraction occurs when the crescendo and decrescendo of the contraction are not mirror images of one another. This relates to unequal relaxation of uterine muscle fibers and the clinical importance is not known.